On Friday the 15th of June, we had the opportunity to present a workshop at the “Giornate degli Specializzandi di Igiene e Medicina Preventiva”. This is an annual congress that brings together all the public health residents in Italy. This year it took place in the beautiful city of Catania, Sicily.
The workshop was organised on the second day of the congress. Alberto, EuroNet’s president, and Spela, E-RECT’s working group lead, presented the session. During the workshop, both euroneters described the network to our Italian colleagues, as well as the work that we do in relation to improving the public health training programmes in Europe.
After a couple of short presentations, the Italian residents were divided in groups and asked to give their opinion about how public health could be promoted as a popular specialty among medical students; and about the good and not so good aspects of their residency programmes. Their responses were discussed and collected, so that they can inform future work of the network.
The workshop proved to be popular, generating useful discussions which prove the importance of the topic.
We were also able to see old euroneters who we hope to see soon and to meet new residents, some of which have been gifted with EuroNet’s party spirit (to be continued in Valencia). We really enjoyed the Sicilian hospitality, which included a large amount of aubergines and late parties.
We want to thank specially Robin Thomas, who was “in charge” of us. He really did a fantastic job and we are very grateful to him.
We hope this is only the beginning of EuroNet’s involvement in national events such as this one. By being present in this type of congresses, we ensure that our work is aligned with the interests of public health residents across all European countries.
Once again, grazie per tutto EuroNet Italy!
EuroNet Summer Meeting – Programme for Valencia 2018
Next EuroNet’s meeting programme is now available.
Registration form: https://goo.gl/D8khgu
Meeting venue: Faculty of Medicine, Avda Blasco Ibañez nº 15, 46010 Valencia
EuroNews MRPH #14
EuroNews #14 has been published!
Enjoy the reading!
EuroNews #14: https://euronetmrph.org/news-newsletter/
“FUNI” Workshop
Thanks to our Italian members, EuroNet has been given the opportunity to organise a workshop at the Giornate degli Specializzandi in Igiene e Medicina Preventiva, which will take place on the 15th of June in the beautiful city of Catania.
Our president Alberto Mateo and E-RECT’s WG lead Špela Vidovič will lead the workshop, titled “FUNI” (Facilitating residents’ mobility, Undertaking research, Networking, Improving residency programmes). For one hour and a half, they will lead a discussion on how training programmes work across Europe; what the strengths and weaknesses of each programme are; how we can improve them and what EuroNet is already doing.
The workshop will be a fantastic opportunity to present and promote our network, as well as some of the work that we are doing, particularly in relation to the E-RECT study and the Professionalisation Working Group.
Our Italian members will be facilitating the workshop, making sure it is a success. They will also be in charge of showing the city to Alberto and Špela, as well as making sure they try some of the finest Sicilian food and wine. Pictures and report will follow the workshop. So, stay tuned!
Residency access in Italy: how did it change?
In Italy, procedures of application in medical residency have been deeply re-elaborated in the last four years. Until 2013, in order to pursue their own careers, young graduate doctors had to choose the University and the affiliated healthcare facility where they wanted to specialize, and take an entree exam there in these structures, through a local competition.
A first fundamental reform took place in 2014, when the introduction of a national competition replaced the hundreds of exams in the different Italian universities. Therefore, candidates were asked to individually choose up to six different branches of medicine, as well as to locate some preferred facilities; after the competition, the Ministry of Education, University and Research (MIUR) issued several national rankings, one for each medical specialization. The examination consisted of a multiple-choice test subdivided into a first general part identical for all, a second one based on three different macro-areas (medical area, surgical area, and area of health services), and a final ten-question test specific to different branches. In the following two years, residency access competitions remained almost unchanged.
Yet, the 2017 edition, albeit being structured along the lines of the previous ones, has been developed following a new regulation adopted by the MIUR on September 6th, with the purpose of streamlining and making the test procedures more transparent. Moreover, access to the different Schools of Specialization is now regulated by an annual national multiple-choice test. This test is the same for all students throughout the country, and it consists of 140 questions about key topics related to Medical School’s programmes, as well as some questions more specific to all the different medical branches.
A single national ranking including all the participants is then drafted based on the test’s scores. Starting from top of the list, each participant doctor who won a place as a resident is contacted in order to let him choose and declare both the preferred school of specialization and the selected city facilities. Each doctor is given the possibility of choosing up to three different kind of residencies, in order of preference. The achievement of high test scores allows to get a good ranking. The final score is calculated by summing the number of correct answers (that are worth 1 point each, while each wrong answer means losing 0.25 a point) to “extra-test” points, represented by University curriculum, which weighs definitely less than it used to in the previous tests ; in fact, now it is less than 7 points – rather than 15 – consisting of: up to 2 points for the degree grade, up to 3 points assigned after the weighted average of university exams’ grades, 0.5 a point per an experimental graduation thesis, and 1.5 points for a previous Ph.D.
Each annual edition of this new modality of residency access has to be specifically addressed by a competition notice published around the month of May.
In conclusion, this new national test was held last November, and, starting from December 4th, the awarded candidate doctors were able to choose the preferred available facilities, in a batch process depending on their score and rank position. The last residents’ allocation was held on December 22nd.
To those who have just started their training activities, all that remains for us to do is to wish you good luck, or if you prefer, buona fortuna!
More details at: MIUR, Italy – www.miur.gov.it
_________________________
Pietro Ferrara
Public Health Resident, University of Campania “L. Vanvitelli”, Naples, Italy
Viola Del Prete
Public Health Resident, University of Campania “L. Vanvitelli”, Naples, Italy
(As published in EuroNews #13)
Public Health Residency: Time for Focus and Opportunity
Last January, I started my residency in Public Health in Oporto, at an institution responsible for all the population living or working in the oriental area of the city. I’m very pleased with my choice and I feel very welcomed by this big community. Fortunately, public health in Portugal is on the rise in the last 8 years with an increase number of all public health professionals. Even in Europe and all around the world, public health is becoming more prominent in order to have real impact in our lives and on the ones in most need. Euronet is an excellent example of the ambition and hard work of a new technological generation of public health doctors, understanding the value of a solid and robust network between different countries and cultures. One of my first goals, after choosing public health as my profession, was to find out what it is and its objectives. Besides its fundamental actions according to WHO, promoting health, preventing disease and prolonging life, and the additional ten major interventions that we can and should address on a daily basis, I read a sentence stated by Arnaldo Sampaio, a reference figure in the development of public health in Portugal, that, in my opinion, describes the range that public health can have, “If you want you can even consider the public lighting as a promoter of better Public Health, since it gives more safety to pedestrians and decreases the probability of road accidents”.
In the first residence year our program in Portugal is focused on community health. A major aim of this phase is to learn and practice epidemiological surveillance and intervention. In Oporto, we work with a population that has a big incidence of tuberculosis comparing with other regions of Portugal. It is characterized for having a low socioeconomic status and poor neighborhoods, and consequently low hygienic conditions and reduced search of healthcare treatment in due time, which are risk factors for acquiring the disease. Those conditions promote the spread of the disease between family, friends and work colleagues. Although our job’s aim is towards the identification of the source of the disease and all the contacts, there are, unfortunately, some barriers and bureaucratic restrictions that not allow us to do it properly. For example, the minimum 6 month period of treatment of tuberculosis is a huge downsize in the battle against the disease, since some cases doesn’t even complete the treatment, despite its mandatory order to do it under observation. One suggestion to fight those problems could be health institutions merely for treating tuberculosis where patients could be hospitalized during it, depending on the danger to themselves or others. We have the ability to, if not eradicate, reduce considerably the incidence of tuberculosis with new and good practices, using all the information that we have available today.
In almost two months I proudly declare that public health is exceeding my expectations, that I feel highly motivated and we all should encourage each other in order to overcome all the barriers that we might face along our path. Public health gives us all the tools to make a better, healthier and more sustainable world. Together, and perhaps with Euronet and its communication assets, we can make the difference.
_________________________
João Paulo Magalhães
MD, Public Health Resident, Portugal
(As published in EuroNews #13)
Public Health Masters in the context of Public Health Resident Training in Europe
Nowadays, large disparities are still present among the different Public Health Masters (MPH) included in the training programmes of public health residents in Spain. Moreover, the impending changes in our training programme may result in a reduction of specific public health training for public health residents from four to two years, with the likely exclusion of MPHs as part of these changes.(1)
The Spanish Association of Residents in Preventive Medicine and Public Health (ARES MPSP) is concerned about these discrepancies and their consequences within the European context. Our aim was to characterize the disparities present among the different public health resident training programmes across the European Countries. A survey was developed to this end.
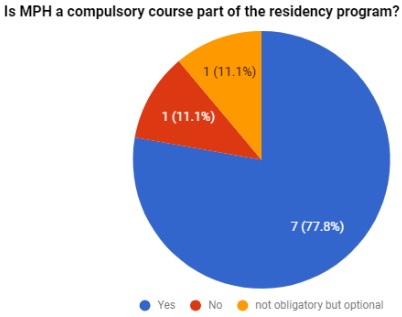
All members present at the Strasbourg meeting, representing eight of the nine countries that are part of EuroNet-MPRH, participated at the survey, which consisted in a single question “Is MPH a compulsory course part of the residency programme?”. Ireland, the remaining country, received the survey via email.
All countries, except Italy and Ireland, declared to have a MPH programme as part of their residency training programme. In Ireland, MPH is optional (See figure 1). Regarding commitment and time-dedication, 33%(3/9) of the surveyed countries reported the presence of part-time MPHs, while 44% (4/9) reported full-time commitment programmes.
Fees are more often covered by the employer then students, except in France, where trainees must sustain the fees by themselves. In three countries costs are covered by the ministry.
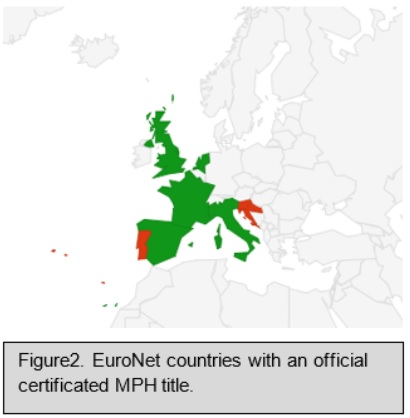
All countries except Portugal and Slovenia have an official MPH title. Although Croatia has an official MPH title, they are unsure about the accreditation status. Schools in Portugal are encouraged to consider MPH programmes as the academic part of a master programme, where students pay an extra fee to present a thesis and to obtain a degree. Slovenia hopes to have one in the future (See figure 2).
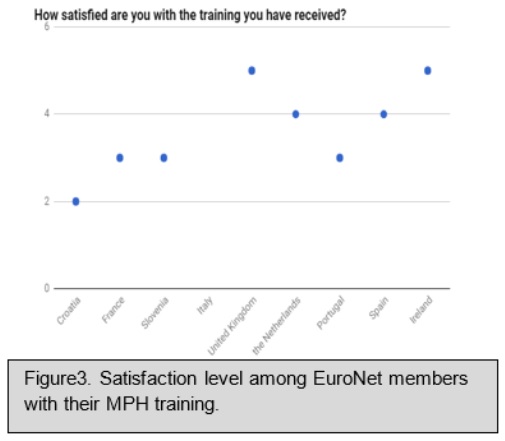
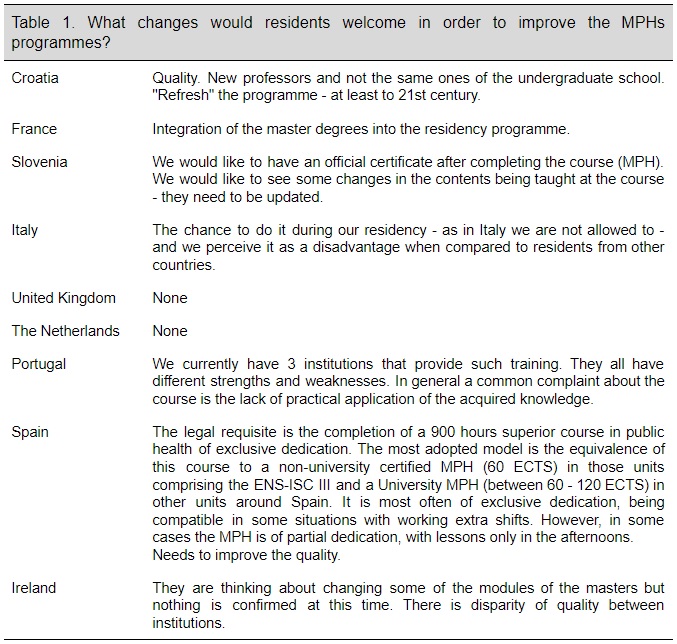
The residents satisfaction with the training received during the MPH was assessed with the question “How satisfied are you with the training you have received?”. The results show a median satisfaction of 3.5 points out of 5 [IQR: 2-5] (See figure 3). Moreover, residents were asked about what kind of changes they would like to observe inside the MPHs programmes (Table 1).
As presented, there are great disparities among different MPH programmes across Europe. It would be desirable to further unify MPH criteria in order to increase training quality and mobility.
_________________________
References
- Inamo J. et al. Existe-t-il des spécificités dans la prévalence et la prise en charge de l’hypertension artérielle aux Antilles-Guyane par rapport à la France métropolitaine ? BEH thématique, 16 décembre 2008 ; 49-50. Romon I. et al. Le poids important du diabète sur la mortalité dans les départements d’outre-mer. InVS, Mars 2007.
- Jaries R. et al. Population movements and the HIV cascade in recently diagnosed patients at the French Guiana -Suriname border., 2017; 13:1-5
- Carde E. Les discriminations selon l’origine dans l’accès aux soins. Access to health care and racial discrimination. Santé publique 2007, volume 19, n° 2, pp. 99-109.
_________________________
Fátima C. Mori Gamarra
Preventive Medicine and Public Health resident at Complexo Hospitalario Universitario de Ourense, Galicia – Spain
Julio Muñoz Miguel
Preventive Medicine and Public Health resident at Hospital Clínico Malvarrosa, Valencia – Spain
Adrían Aginagalde Llorente
Preventive Medicine and Public Health resident at Hospital Universitario de Cruces – Spain
(As published in EuroNews #13)
French Guiana – Who is the stranger?
In France, as residents, we have the possibility to do a maximum of three rotations in a different place from the one where we are doing our residency. One lazy autumn evening I went through the list of the available rotations in French overseas departments, and I chose Saint-Laurent du Maroni, French Guiana. The choice was simple: a 37 years-old public health doctor had opened a whole public health department in Western French Guiana hospital 5 years before, just out of her residency, while getting a PhD with a thesis on migrants’ health. I could not ask for anything better.
French Guiana is a French overseas department, a former penal colony, wedged between Brazil and Suriname. It is a European outermost region and the only border of Europe with South American countries, it hosts a European spaceport from where Ariane rockets are launched every month and, of course, Euro is the currency.
I vaguely imagined what expected me. I read the data: the epidemiological profile of the region is similar to that of developing countries, where communicable diseases like dengue fever and leishmaniasis persist alongside a high prevalence of cardiovascular diseases and diabetes. HIV is epidemic (>1%), half of the population is less than 25 years old and the fertility rate is 3.5%.
The first thing I noticed when I arrived in Saint-Laurent, which has more than 40 thousands inhabitants and lies on the shore of the Maroni river, was the lack of public transportation. Being born and bred in cities, public transportation for me is a fundamental part of the landscape and the absence of it struck me immediately. Public transportation has practical implications, but also a symbolic meaning. It carries communities together and fights geographical isolation. In its absence, people living in the peripheries are left out of the public life. They cannot easily access services, which are historically aggregated in the city center. It did not take long to discover that isolation, lack of access to services, inequalities, structural discrimination would be key words of my experience here.
I participate in most of the activities of the public health department, whose mission spaces from prevention activities – an IST clinic, therapeutic patient education for chronic illnesses, cultural mediation, school interventions on sexual health… – to research and training, to international cooperation with neighboring Suriname, to providing medical missions to the health centers along the Maroni river. This allows me to have a glance at population needs and the difficulties to tackle them.
There is no single cause for the particular obstacles that may be encountered in health care in French Guiana. Part of the problem are practical issues: the scarcity of means – In terms of money but above all in terms of human resources – , the complexity of the territory – the road stops 50 km south of Saint-Laurent and you can only reach further towns by boat or by plane -, the distance from the capital city, where decisions are taken.
However, it is not as straightforward as that. Working in this environment is the concrete exemplification of how determinants of health act.
Here, as professionals or laypeople, we are obliged to confront with theoretical and political questions that we do not usually think about in our day-to-day life, such as the subject of decentralization, the role and responsibilities of the State, the scars of colonialism, how societies form and develop. Questions arise about migrations and nationality3. We wonder who is a foreigner, is it the person who was born here but who does not speak French, is it the person who comes from across the river, is it the Parisian doctor, is it me, is it no one or are we all?
And the list of questions continues. How can we support sexual violence survivors, which can be count in hundreds every year? What is the best way to advocate for undocumented migrants and to provide appropriate services to mobile people? How do you tackle the complex ties between health, education, (lack of) job opportunities, social structures? What about indigenous population?
I do not have simple answers. However, I had the great opportunity to combine practice and reflection and to learn from dedicated professionals and for that I am grateful. I hope I leave you craving for more French Guiana.
_________________________
References
- Inamo J. et al. Existe-t-il des spécificités dans la prévalence et la prise en charge de l’hypertension artérielle aux Antilles-Guyane par rapport à la France métropolitaine ? BEH thématique, 16 décembre 2008 ; 49-50. Romon I. et al. Le poids important du diabète sur la mortalité dans les départements d’outre-mer. InVS, Mars 2007.
- Jaries R. et al. Population movements and the HIV cascade in recently diagnosed patients at the French Guiana -Suriname border., 2017; 13:1-5
- Carde E. Les discriminations selon l’origine dans l’accès aux soins. Access to health care and racial discrimination. Santé publique 2007, volume 19, n° 2, pp. 99-109.
_________________________
Maria Francesca Manca
Public Health Resident, France
(As published in EuroNews #13)
Noncommunicable diseases in humanitarian settings

In the 21st century, we live in a world regularly affected by emergencies, often with severe local and regional health consequences. In the context of climate change and corrosive political instability in many world regions, it is probable that we will see an increase in disasters or their resulting health impacts.1 By the end of 2016, 65.6 million people worldwide were forcibly displaced from their homes. The record number includes 22.5 million refugees, 2.8 million asylum seekers and 40.3 million people living in internal displacement (ID).2,3
The number of ID has nearly doubled since 2000 and has increased sharply over the last five years. For displaced populations health care has traditionally focused on maternal and child care and treatment of communicable diseases. While these traditional health priorities remain relevant, demographic and lifestyle changes are increasing the burden of noncommunicable diseases (NCD) in populations worldwide. This epidemiological shift poses new challenges for humanitarian agencies and host country governments. NCD accounted for 19% to 46% of mortality in the top 5 source countries for refugees in 2015.4
In the absence of regular care and access to medications, NCD may result in complications requiring costly specialised care and have the potential to seriously compromise both quality of life and life expectancy, since the risk of exacerbating pre-existing conditions or suffering acute complications, is two to three times higher than it was beforehand. In the initial response of an emergency management of NCDs should focus on treatment of life-threatening or severely symptomatic conditions. During the recovery phase after emergencies or during protracted emergencies such as long-term settlements, the management of NCDs should be expanded to include management of sub-acute and chronic presentations. WHO recognizes the growing problem of NCDs, and in 2013 introduced the Package of Essential Noncommunicable Disease Interventions, or WHO PEN, a set of tools to early detect and manage cardiovascular diseases, diabetes, chronic respiratory diseases and cancer in order to prevent life-threatening complications, such as myocardial infarction, stroke, kidney failure, amputations and blindness.5
There is a need to identify challenges and gaps in order to create a more holistic approach to effective planning, implementation and delivery of health care services to displaced populations with chronic NCD.
_________________________
References
- Demaio, A., Jamieson, J., Horn, R., de Courten, M., & Tellier, S. (2013). Non-Communicable Diseases in Emergencies: A Call to Action. PLoS Currents, 6, 5-23.
- UNHCR (2017). Global Trends – Forced Displacement in 2016. United Nations High Commissioner for Refugees, Geneva.
- IDMC (2017). Global Report on Internal Displacement. Internal Displacement Monitoring Centre, Geneva.
- Sethi, S., Jonsson, R., Skaff, R., & Tyler, F. (2017). Community-Based Noncommunicable Disease Care for Syrian Refugees in Lebanon. Global Health: Science and Practice, 5(3), 495–506.
- WHO (2010).Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings. World Health Organization, Geneva
_________________________
Ana Pinto de Oliveira
2nd year Public Health Resident
ACES Arco Ribeirinho, Barreiro, Portugal
Catarina Neves Oliveira
Public Health Specialist
ACES Arco Ribeirinho, Barreiro, Portugal
(As published in EuroNews #13)