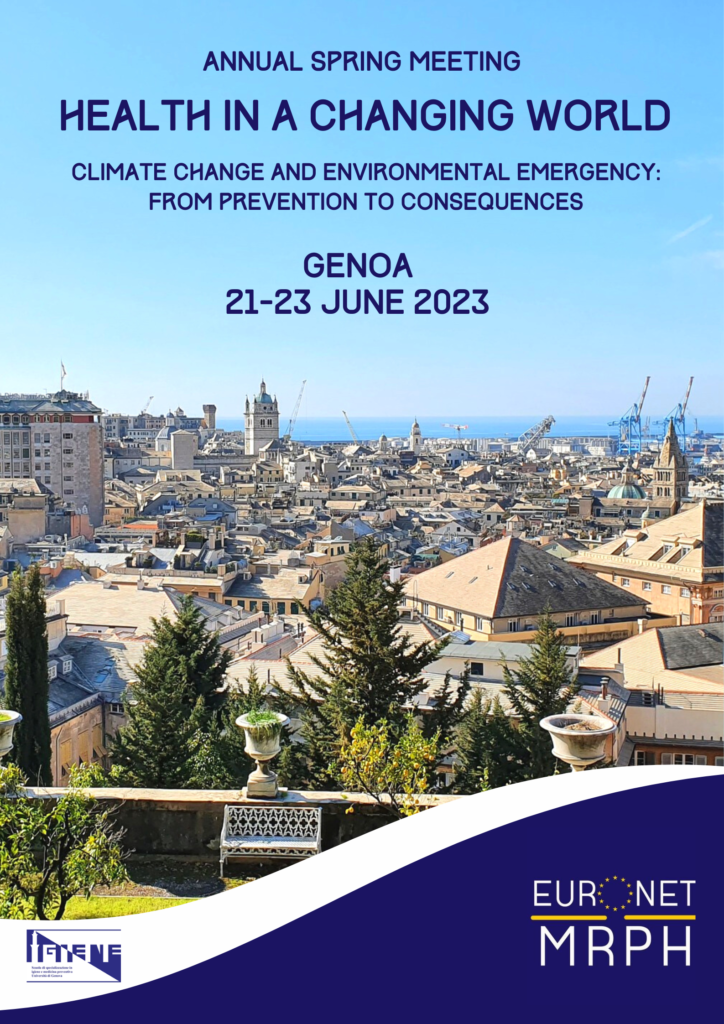
Join us in Genoa, Italy, on June 21-23 for the 2023 edition of EuroNet’s Spring Meeting! The congress is organized by the Organizing Committee of the School of Hygiene and Preventive Medicine of the University of Genova in collaboration with EuroNet MRPH Board and Leads.
This year’s theme is:
HEALTH IN A CHANGING WORLD
Climate change and the environmental emergency: from prevention to consequences.
Our generation is facing a devastating and imminent crisis that cannot be ignored. Increasing extreme weather phenomena are already having catastrophic consequences on our planet and its living beings, and are expected to have profound effects on societies worldwide.
With the help of amazing international speakers, the Spring Meeting 2023 will be an opportunity to explore future public health challenges in a changing world, including environmental degradation, mental illnesses, emerging infectious diseases, migration, climate change communication in public health, and global inequities in the face of the climate crisis. Through our plenary sessions, workshops, and debates, we will also discuss possible ways forward and the frameworks that might guide Public Health in that direction, including One Health and Circular Health.
Genova-Program
download as pdf
SOCIAL PROGRAM
We are working to ensure you have the best time in Genoa and get the opportunity to meet and mingle with fellow colleagues from across Europe! On June 21st, we will break the ice with a free dinner together. Options for June 22nd will be announced soon, but possibilities include music and dinner in a castle (yes, that’s right) or a disco night (dinner included). We recently sent out a survey to investigate which one attracted you more and are now assessing overall preferences.
CONGRESS REGISTRATION
To help us arrange the Spring Meeting’s logistics, please pre-register for the congress (closes on March 23rd). Please pay special attention to spelling your email address correctly in this phase. The email address you provide will be used to send you the link for the official registration at a later stage. Both pre-registration and official registration for the Spring Meeting are free (during the official registration, a fee might be asked for some parts of the social program only).
Update 5/04: Over 200 pre-registrations already, thank you! Missed pre-registration? Don’t worry, official registration opens after the Easter break. Stay tuned!
Update 29/04 : Registration is now open !
Update 09/06 : Registration is closed. We are delighted to announce that we have reached the maximum capacity of 250 attendees. Thank you all for your support.
See you in Genoa
Questions and help : eurogenova2023@gmail.com.
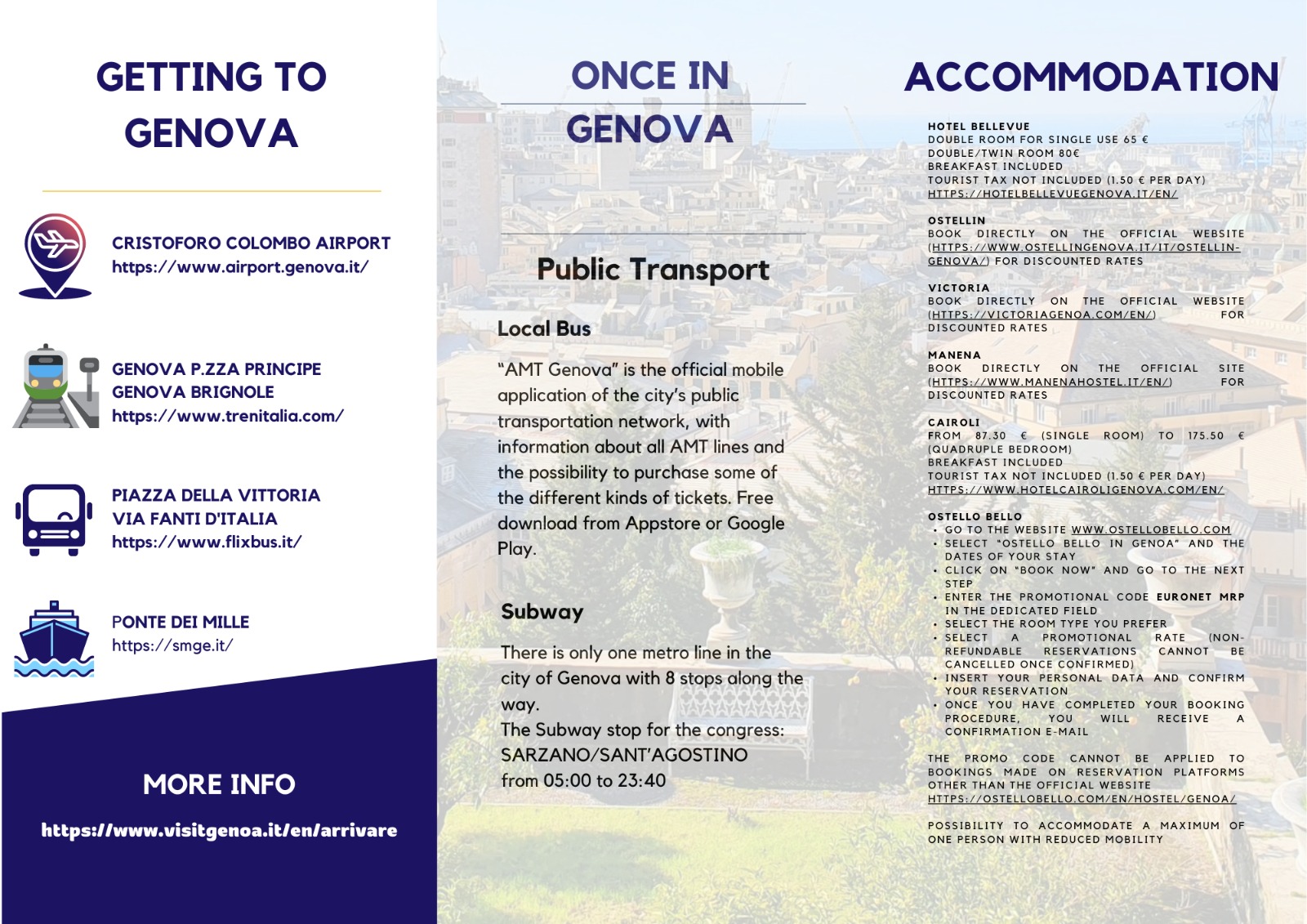
PRACTICAL INFORMATION
ESC – EuroNet Scientific Contest
The Spring Meeting will be hosting the European Scientific Contest (ESC). You may want to seize the opportunity to share and present your research work in Public Health to an international audience including speakers and European residents. Winner gets a free ticket for the 2024 Spring Meeting ! Learn more
Abstract submission is closed