The SAGE Working Group on Vaccine Hesitancy defined vaccine hesitancy as ‘the delay in acceptance or refusal of vaccination despite availability of vaccination services. Vaccine hesitancy is complex and context specific, varying across time, place and vaccines. It is influenced by factors such as complacency, convenience and confidence’ (1). Indeed, it is complex and the reasons cited in the literature are varied, from fears about vaccine safety, worries about ‘overloading’ the child’s immune system, distrust of the pharmaceutical industry and collective amnesia regarding the dangers of vaccine preventable diseases (2). Many parents, unfamiliar with diseases like tetanus and meningitis, make incorrect conclusions when it comes to calculating the risk-benefit of vaccinating their children.
The current measles outbreak in Europe is the direct result of vaccine hesitancy. 13,234 cases have been reported across Europe since July 2017 (3). Sadly, there were also 18 deaths due to measles in this period (3). In Ireland, we have had 76 cases of measles in 2018 so far, with an ongoing outbreak in Dublin as I write this. What can we do to end this outbreak and prevent the resurgence of other vaccine preventable diseases?
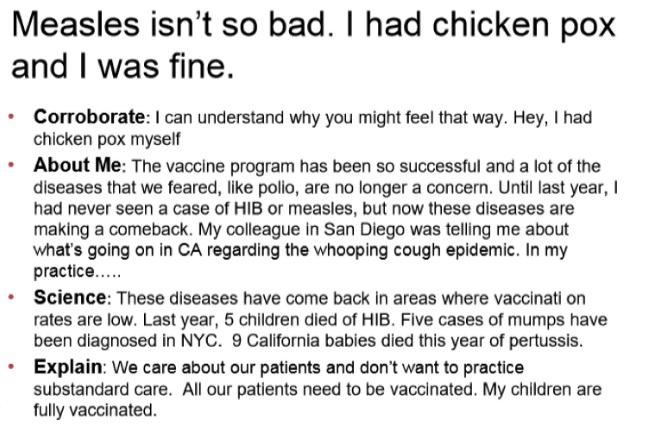
Reviewing the current evidence on what can be done to address vaccine hesitancy is not particularly inspiring. Reminders, whether they are telephone, text or postal, and family incentive rewards have been proven to increase vaccine uptake, but there is limited evidence that they work for vaccine-hesitant individuals (4). A trusted health care professional can also have an impact on changing parental attitudes, but the evidence for the various communication tools that have been designed as aids for these professionals to use is mixed (4). More research and better measurement of outcomes is needed in this area (4). It is not enough just to measure change in attitude to vaccines, we must see if this change in attitude actually leads to increased vaccine uptake.
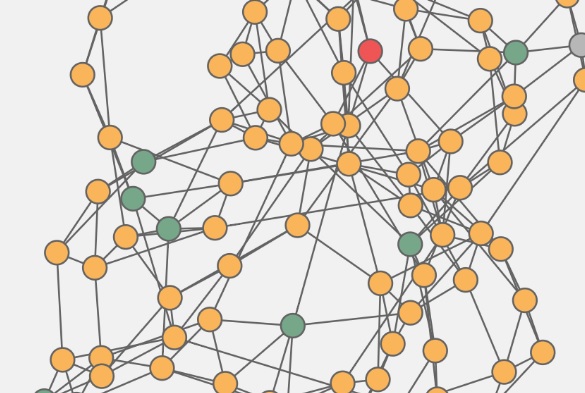
There are advocates for more innovative approaches. Some argue that social marketing frameworks could provide solutions (5). Others propose that children should be taught positive messages about vaccinations in school, as part of their health education, science or even citizenship classes, in order to ‘inoculate’ them against vaccine hesitancy in the future (6). A friend of mine, who teaches teenagers, created a lesson to teach her students critical analysis skills, using information on the benefit and safety of HPV vaccination. These kind of skills are vital for navigating the ‘fake news’ widespread on social media. For younger children, there are online games demonstrating how vaccines work (7). One review found 16 different games in 2016 (7). I lost 20 minutes trying to stop an outbreak with rapid vaccination at this particular link: https://vax.herokuapp.com/game
It’s a little bit addictive! Could positive attitudes to vaccines be engrained at a young age using these methods?
A mixture of targeted interventions to deal with parents in the midst of today’s crisis, as well as methods targeting future generations, will be necessary to tackle this complex issue. It is time to try new approaches. Please contact me at laura.heavey@hse.ie, if you know of any innovative methods to improve vaccination rates that are ongoing in your country
_________________________
References
- MacDonald NE, the SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015; 33:4161–4164
- Marti M, de Cola M, MacDonald NE, Dumolard L, Duclos P. Assessments of global drivers of vaccine hesitancy in 2014 Looking beyond safety concerns. PLoS ONE. 2017; 12(3):e0172310.
- European Centre for Disease Prevention and Control. Monthly measles and rubella monitoring report. Stockholm: ECDC; 2018
- Dube E, Gagnon D, MacDonald N. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine. 2015; 33: 4191-4203.
- Nowaka GJ, Gellinb BG, MacDonald NE, Butler R, the SAGE Working Group on Vaccine Hesitancy. Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine. 2015; 33:4204–4211
- Wilson K, Atkinson K, Crowcroft N. Teaching children about immunization in a digital age. Human Vaccines & Immunotherapeutics. 2017; 13 (5):1155–1157.
- Ohannessian R, Yaghobian S, Verger P, Vanhems P. A systematic review of serious video games used for vaccination. Vaccine. 34 2016; 34: 4478–4483.
_________________________
Laura Heavey
Specialist Registrar in Public Health Medicine
Department of Public Health, HSE, Sligo, Ireland